Katrin Olavessen-Holt, PharmD, CPGx
Autoimmune diseases require close oversight to avoid disease progression, and no one understands that better than those who live with it. While healthcare professionals play a role in avoiding significant side effects, there are a few that often get overlooked. This article focuses on six common mistakes lupus patients make that influence disease progression and quality of life.
- Sun exposure. Photosensitivity is a major problem for people living with lupus. Ultraviolet rays, whether from the sun or artificial sources such as fluorescent lights and halogen bulbs, elicit skin reactions in the form of rashes and/or sores in up to 70% of people with lupus. Additionally, photosensitive reactions may trigger other symptoms like fever, joint pain, flu-like symptoms, fatigue, and even organ inflammation, such as in the kidneys.1,2
Tips: Use broad spectrum sunscreen at the highest level tolerable (70+ spf recommended) with UVA + UVB protection. Apply as directed and apply often. Every two hours outside and every four hours while inside but administer waterproof sunscreen more frequently while in water or sweating. Moreover, apply 30 minutes prior to heading outside. Also, make sure to cover tips of ears, nose, cheeks, back of neck, backs of hands, upper chest, and neck, which are often overlooked.2,3

- Smoking and efficacy of antimalarials and biologics (belimumab). Hydroxychloroquine, an antimalarial, is considered the drug of choice for all people diagnosed with lupus.4 However, people who smoke face exacerbations of disease flares, difficulty controlling disease flares, and may lead to secondary complications. Additionally, evidence suggests smoking decreases the effectiveness of antimalarials, which is directly linked to disease activity.5-7
Tips: If ready to quit smoking, ask a healthcare professional about nicotine replacement (short-acting sprays, gum, and lozenges) and/or long-acting medications like the nicotine patch, maybe even used in combination, for help in smoking cessation. Ask for a plan, set a date, and get started.8
- Methotrexate medication interactions. Another medication commonly prescribed in lupus is methotrexate. As an effective immunosuppressant, methotrexate is used in conjunction with antimalarials and glucocorticoids when disease activity remains uncontrolled. However, it interacts with a slew of other medications (see Table 1 for interactions), including some antibiotics, which most people will encounter in their lifetimes.9-11
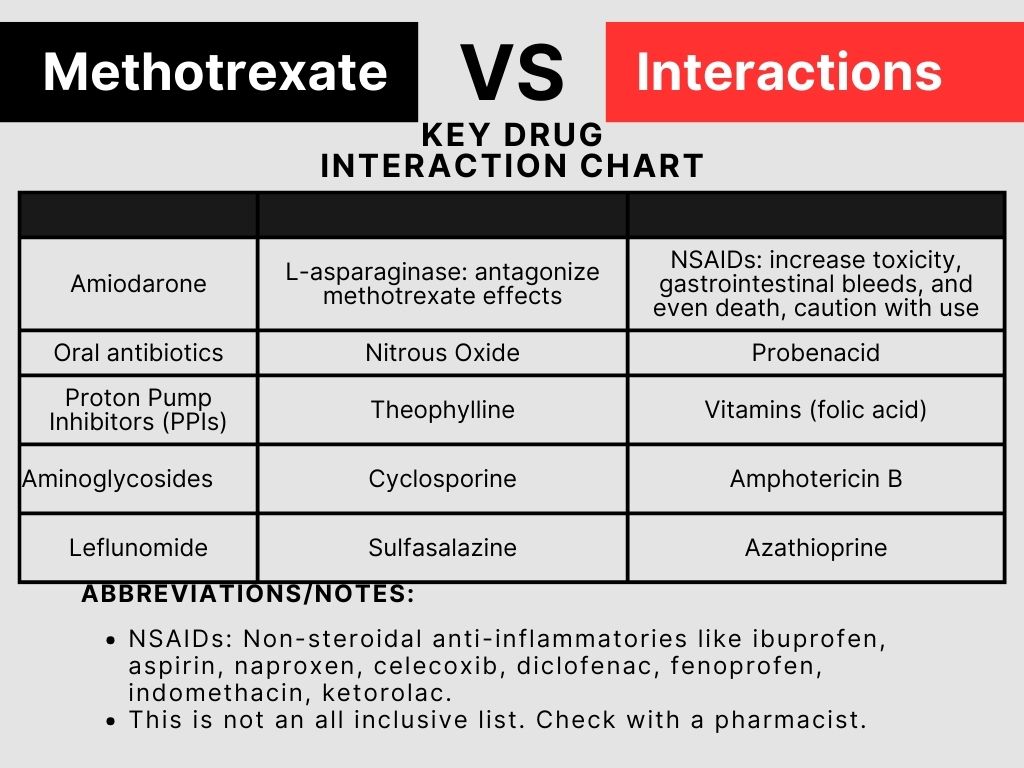
Tips: Ask the prescribing healthcare provider about any interactions when prescribed new medications. Also, question the pharmacist when picking up the prescription about any food or medicine interactions as well. Moreover, keep a list of methotrexate drug interactions and check whenever starting a new medication. An ounce of precaution is priceless.
- Methotrexate, NSAIDs, Antibiotics, and photosensitivity. It is well known that sun exposure in lupus leads to higher disease activity and flares. However, many do not understand that certain medications can and do cause phototoxic, and photoallergic reactions when exposed to UVA light. Therefore, it is important to keep these medications in mind when prescribed or using over-the-counter (OTC).12,13
Tips: When starting any new medication, ask about photosensitivity. Also, wear sunscreen with SPF 30+ (70+ if possible with titanium dioxide or zinc oxide preferred), wide-brimmed hats, gloves, and wear tight-knit long-sleeved shirts and pants to block UVA rays. If able, purchase UV-protected clothes. Also, avoid direct sunlight between 10am to 4pm when effects are strongest. Lastly, ask a pharmacist about interactions with ALL OTC medication purchases.
- Incorrect methotrexate. In rheumatic diseases, methotrexate is prescribed as a once weekly dose. However, it is a common mistake for people to take it daily, which leads to toxicity and even death.14
Tips: Double-check prescription instructions and confirm with a pharmacist. Use a weekly pill organizer to avoid confusion. Ask the pharmacist to only fill a month at a time. Set a day of the week with the pharmacist and doctor for methotrexate ingestion each week.
- Medication Adherence. Everyone forgets at times, but consistent lapses in taking prescribed medication, or even stopping altogether due to cost, side effects, or simply feeling better can all increase disease activity and progression. Additionally, there are withdrawal effects associated with certain prescriptions.15
Tips: Consider a pill organizer to keep track of medications and their timing. Use apps or set daily timers on phones as a reminder. Always speak with a doctor before stopping a medication, even if feeling better. If a dose is missed, always speak with a pharmacist for guidance on when to take it next.
Paying attention to these six common mistakes helps deter disease flares and poorer outcomes. By staying aware of sun exposure effects, smoking effects, drug interactions, medication photosensitivity effects, incorrect dosing, and medication adherence, people can avoid risks and improve quality of life. As always, when in doubt, ask a healthcare professional.
If you need a medical writer with pharmacist expertise, contact me at innovationsmedicationmgmt@gmail.com.
References:
- Ji Hyun Sim, Ambler WG, Sollohub IF, et al. Immune Cell–Stromal Circuitry in Lupus Photosensitivity. Journal of Immunology. 2021;206(2):302-309. doi:https://doi.org/10.4049/jimmunol.2000905
- Tips for managing sensitivity to light | Lupus Foundation of America. http://www.lupus.org. https://www.lupus.org/resources/tips-for-managing-sensitivity-to-light
- American Academy of Dermatology Association. How to apply sunscreen. http://www.aad.org. Published 2024. https://www.aad.org/public/everyday-care/sun-protection/shade-clothing-sunscreen/how-to-apply-sunscreen
- Georgia-Savina Moysidou, Antonis Fanouriakis. EULAR 2023 Recommendations for the Management of Systemic Lupus Erythematosus: One Step Forward. Mediterranean Journal of Rheumatology. 2024;35(1):63-63. doi: https://doi.org/10.31138/mjr.130124.erm
- François Chasset, Camille Francès, Stéphane Barete, Zahir Amoura, Laurent Arnaud. Influence of smoking on the efficacy of antimalarials in cutaneous lupus: a meta-analysis of the literature. J Am Acad Dermatol. 2015 Apr;72(4):634-9. doi: 10.1016/j.jaad.2014.12.025. Epub 2015 Jan 30. Erratum in: J Am Acad Dermatol. 2015 Aug;73(2):353. PMID: 25648824.
- Georges El Hasbani, Madi M, Sadek A, Srour L, Uthman I, Jawad AS. The Impact of Tobacco Smoking on Systemic Sclerosis, Idiopathic Inflammatory Myositis, and Systemic Lupus Erythematosus. Clinical Medicine Insights Arthritis and Musculoskeletal Disorders. 2024;17. doi:https://doi.org/10.1177/11795441241290522
- Shawn G Kwatra. Toll-like receptor-9 signaling and decreased efficacy of antimalarial drugs in smokers with cutaneous lupus erythematosus. Journal of the American Academy of Dermatology, Volume 73, Issue 2, e79
- Mayo Clinic Staff. Quit-smoking products: Boost your chance of success. Mayo Clinic. Published 2017. https://www.mayoclinic.org/healthy-lifestyle/quit-smoking/in-depth/quit-smoking-products/art-20045599
- CL Ronchera, T Hernández, JE Peris, F Torres, L Granero, NV Jiménez, JM Plá. Pharmacokinetic interaction between high-dose methotrexate and amoxycillin. Ther Drug Monit. 1993 Oct;15(5):375-9. doi: 10.1097/00007691-199310000-00004. PMID: 8249043.
- Karine Titier, Fabrice Lagrange, Fabienne Péhourcq, Nicholas Moore, Mathieu Molimard. Pharmacokinetic interaction between high-dose methotrexate and oxacillin. Ther Drug Monit. 2002 Aug;24(4):570-2. doi: 10.1097/00007691-200208000-00018. PMID: 12142645.
- METHOTREXATE, VIALS (methotrexate, vials) 9 Drug Interactions | Pfizer Medical Information – Canada. Pfizermedicalinformation.ca. Published 2025. Accessed March 6, 2025. https://www.pfizermedicalinformation.ca/methotrexate/drug-interactions
- Safety update: methotrexate and photosensitivity reactions. Drug and Therapeutics Bulletin. 2023;61(12):179-179. doi: https://doi.org/10.1136/dtb.2023.000056
- Delarue-Riffel R. Sun Exposure, Medications and Rheumatoid Arthritis. Arthritis Research Canada. Published November 30, 2017. https://www.arthritisresearch.ca/sun-exposure-medications-and-rheumatoid-arthritis/
- Methotrexate once-weekly for autoimmune diseases: new measures to reduce risk of fatal overdose due to inadvertent daily instead of weekly dosing. GOV.UK. https://www.gov.uk/drug-safety-update/methotrexate-once-weekly-for-autoimmune-diseases-new-measures-to-reduce-risk-of-fatal-overdose-due-to-inadvertent-daily-instead-of-weekly-dosing
- Laura-Alexandra Anghel, Andreea Maria Farcaş, Radu Nicolae Oprean. Medication adherence and persistence in patients with autoimmune rheumatic diseases: a narrative review. Patient Prefer Adherence. 2018 Jul 3;12:1151-1166. doi: 10.2147/PPA.S165101. PMID: 30013327; PMCID: PMC6037147.
