by Katrin Olavessen-Holt, PharmD, CPGx, CMTM, BA Psych
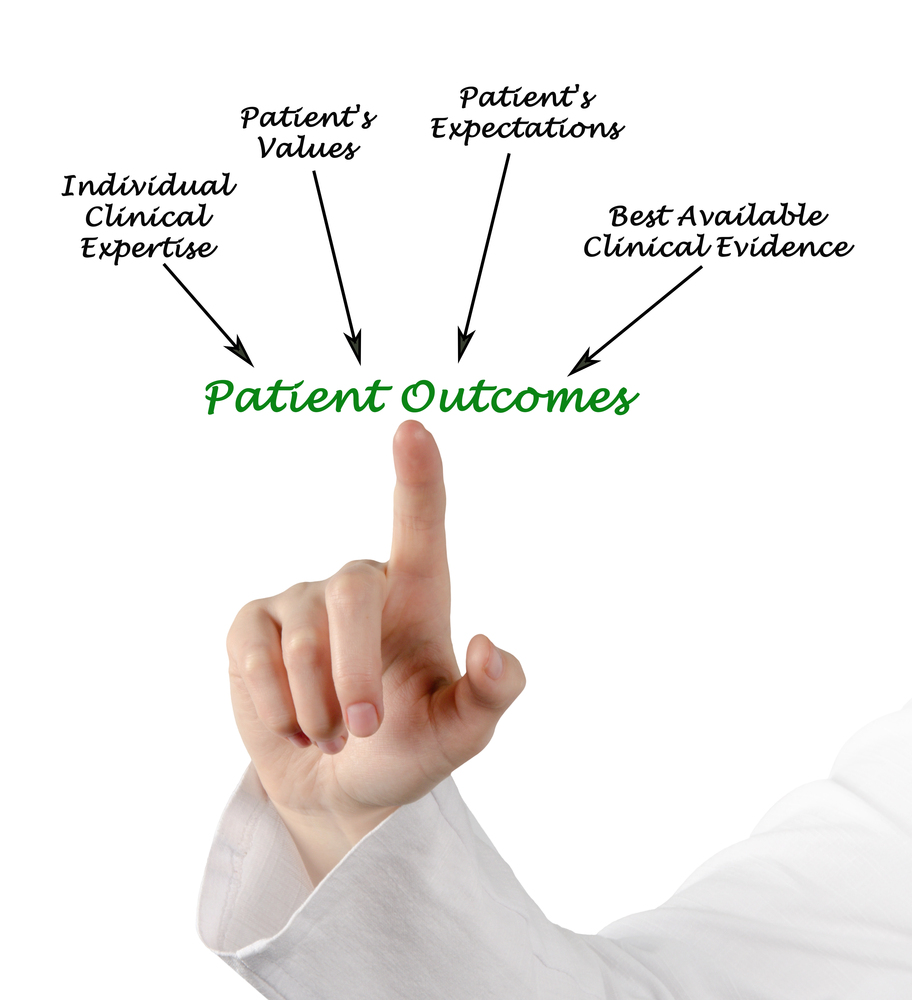
When it comes to managing chronic autoimmune diseases like lupus, patient-reported outcomes in rheumatology are finally getting the attention they deserve. In this week’s episode of The Wellness Pharmacist with Dr. Kat, we explore a powerful new study published in the Journal of Clinical Rheumatology (Feb 3, 2025) that dives into how patients’ voices can actually predict health-related quality of life better than lab results alone.
Here’s the thing—too often, patients are told they’re “fine” because their labs are normal, yet they still feel exhausted, foggy, and unwell. This study confirms what many of us have been saying all along: doctors and patients don’t always see eye to eye, especially when it comes to invisible symptoms like fatigue.
We talk about why that disconnect happens, and how patient-reported outcomes in rheumatology can help bridge the gap between clinical numbers and real-life quality of life. These tools give patients a structured way to report how they feel day to day, which can be just as important, if not more, than what’s in their chart.
Listener Kim asks, “How can I get my doctor to take me seriously when my labs are normal, but I feel awful?” I share tips for starting that conversation and bringing PRO tools to your next appointment.
If you’re living with autoimmune disease and feel unseen or unheard, this episode is for you.
🎧 Listen now and check out more autoimmune health insights at www.innovationsmedicationmanagement.com
🌟 And don’t miss my upcoming mini course, Fatigue Fix—a realistic guide to energy management when you live with autoimmune fatigue. Coming soon!
SUBSCRIBE
To get updates on podcasts, coaching tips, etc… please subscribe to the newsletter here!
YouTube
Watch it on Innovations Medication Management YouTube channel here!